Enough of the errors – we need courageous people to take truly courageous steps to stop healthcare worker harms – Part 2
This is the second part of a blog by our infection prevention and control advisor, Dr Evonne T Curran. In the second half of this blog Evonne continues to describe the truly courageous steps we need decision-makers to take to protect healthcare workers from harm.
Truly Courageous Step 6 – Adopt High-Reliability Theory – Deference to Expertise
There were four arms to protect HCWs and initially they all got it wrong and possibly reassured themselves that as they were of the same opinion, they must be correct:

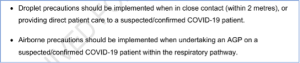
Figure 1: Definitions from the Scottish Literature Reviewers
The four arms which should independently and collectively have prevented so much harm, considered themselves experts and not in need of additional expertise. Deference to expertise is a high-reliability characteristic and not a weakness. However, despite knocking on the door the real experts (aerosol scientists) were not allowed in.
Truly Courageous Step 7 – Consider what failure would look like – then look to see if it is happening
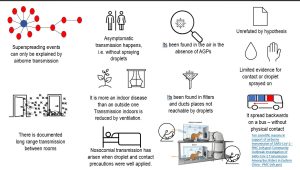
Another high-reliability characteristic is a “preoccupation with failure”. Such an approach would mean identifying what would happen if the assumptions of transmission were wrong and then looking to see if these indications were present. Had they done so, they would have seen evidence of their errors, e.g., transmission outwith AGPs, transmission arising when droplet precautions were being well applied, transmission which could only have been airborne, (superspreading events, asymptomatic transmission, transmission in a cinema over 3 sittings, etc., etc [Figure 2]). However, there was no high-reliability approach, they did not create a picture of what failure would look like, so when it appeared, it went unrecognised.

Figure 2: 10 scientific reasons covid is airborne
Truly Courageous Step 8 – Deploy systems to stop the perpetuation of errors
The 25 Scottish literature reviews failed to identify the correct mode of transmission. They erroneously concluded that the mode of transmission was through “Close Contact” – which is not a mode of transmission – it is a space wherein transmission happens. Alongside this was the phrase “mediated by respiratory particles”. This was unhelpful because the term is omitted from their glossary and there are no “Respiratory Particles” Precautions.

Decision-makers either failed to recognise the need for change or repeatedly decided not to admit to errors and deploy safety. A plan to ensure the prevention of error perpetuation is needed.
Truly Courageous Step 9 – Continuously update the situation awareness to reflect new and changing risks
Situation awareness comprises 3 questions to enable optimal decision making:
- Perception: What is happening?
- Comprehension: So what?
- Prediction: What will happen next if nothing changes?
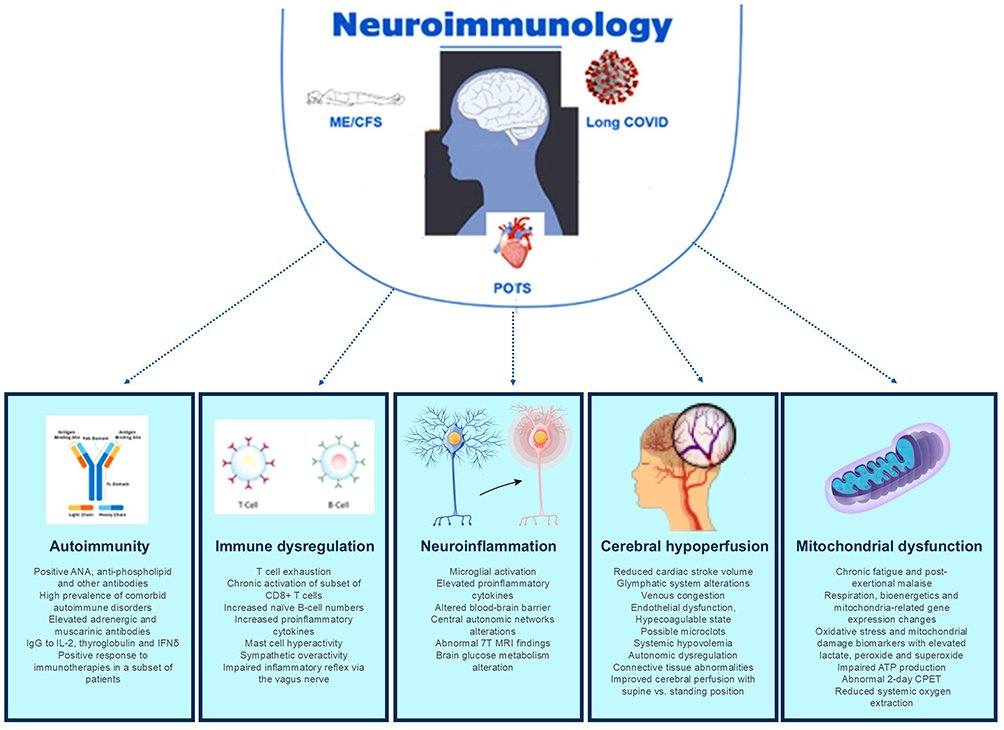
COVID is no longer the acute threat it was. It is now more insidious, and it causes chronic and acute harms – but not always in the lung. It affects any and every organ, including the brain, the heart and blood vessels. The more infections the greater the risk of long-term disability. Clearly, a ‘carry-on harming’ approach is unsafe decision-making, and an updated and accurate situation awareness is urgently needed.
Truly Courageous Step 10 – Acknowledge failures of oversight and again put high-reliability theory into practice
Everyone in the NHS is overseen by somebody. Yet, the Infection Prevention and Control Networks (IPCNs) were left unchecked and uncorrected. I, like many others, wrote and provided evidence of errors in definitions, interpretation and decision-making to those who oversee IPC guidance writers. Oversight should have prevented much harm – why this was not effective during the period of the biggest ongoing HCW injury is inexplicable. Never again should such decisions be made without sufficient and frequent oversight.
Comment
 There will always be errors – look for them, admit they have occurred and make it safe, i.e., change the guidance. In August 2024, Scotland produced an updated Transmissions Based Precautions literature review. In this review they acknowledge the fact that the model they had been using of droplet/aerosol was “inadequate”. They acknowledged that the WHO had had no evidence to support their assertion of how AGPs turn droplet spread infections into airborne ones. And yet 7 months later the guidance remains uncorrected – its still droplets unless AGPs….
There will always be errors – look for them, admit they have occurred and make it safe, i.e., change the guidance. In August 2024, Scotland produced an updated Transmissions Based Precautions literature review. In this review they acknowledge the fact that the model they had been using of droplet/aerosol was “inadequate”. They acknowledged that the WHO had had no evidence to support their assertion of how AGPs turn droplet spread infections into airborne ones. And yet 7 months later the guidance remains uncorrected – its still droplets unless AGPs….
Improved safety so that everyone can recognise the airborne risks in clinical spaces, e.g., where the ventilation is poorest, where transmission happens most, what prevention will achieve the greatest results can only happen once the above 10 Truly Courageous steps are taken. In this country we allowed innocent Post Masters and Mistresses to go to jail, we gave infected blood knowing it was infectious. And now we must own up that we infected HCWs due to adherence to erroneous assumptions of safety. My last years in the NHS were ones following a High-Reliability approach. It was searching for errors, finding them and preventing future ones. The decision-makers made errors that caused harms. I and many others plead for the implementation of 10 truly courageous steps to stop harms and build a safer NHS.



 There will always be errors – look for them, admit they have occurred and make it safe, i.e., change the guidance.
There will always be errors – look for them, admit they have occurred and make it safe, i.e., change the guidance.