In Part 2 of her latest Blog, Evonne T Curran continues to reflect on how infection prevention and control guidelines evolved and how errors and flaws continued to be included.
Part 1 of the blog can be accessed by clicking here.
Lack of IPC oversight grew
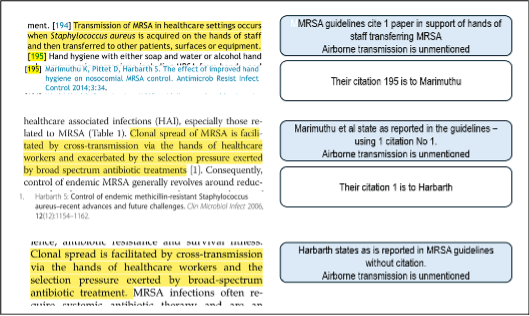
As guidance writers became ever more distant from the ‘IPC coalface’, over time the lack of infection prevention and control (IPC) oversight grew. There was a deference to connoisseurship (i.e., to guidance writers and guidance producing organisations). Also, as evidence-based guidelines contained hundreds of citations they became impenetrable to IPC professionals and were taken to be correct rather than subject to detailed examination for errors. A default to hand transmission and a diminution of the importance of airborne dissemination became evident (See Figure 1). Thus, IPC awaited a pandemic, they predicted would happen, with respiratory guidance that “defied physics”. I was there – mea culpa.
Figure 1: “Evidence based guidelines” showing an absence of recognition that airborne dissemination exists, and providing minimal evidence for hands being responsible for MRSA transfer
The mode of transmission as reported in national manuals is “contact”. People with non-resistant S. aureus do not require isolation even if they have abscesses or the conditions listed above.
Let’s change the guidelines and the IPC manuals to accept evidenced Modes of Transmission
Respiratory guidelines all contained errors and flaws
Respiratory guidelines in national manuals, from professional societies and from the WHO all contained errors and flaws. This is not the issue. Guidelines are produced by people and people make mistakes. Which is exactly why clinical colleagues had been developing procedures for preventing errors for over 30 years. However, these skills are absent in IPC guidance writing. Rather than actively looking for errors, learning from them, and adopting procedures to prevent them, IPC have denied their existence – merely changing words – but without addressing the issue of how the error arose.
The World Health Organisation took two years to acknowledge the airborne transmission of Covid-19
The WHO took 2 years to acknowledge airborne transmission during a pandemic – the two years when the impact on people and care settings was at its peak. The error’s cause was never explained. It is unsafe to consider or accept any individual or organization as being error-proof – even the WHO. For example, there has been no acknowledgement that it was improper for the WHO’s pandemic planning guidance to state they did not know the implications of the difference between aerosols or droplets. They should have found out – the aerosol scientists knew. In another unexplained error the WHO used citations to bolster their hand hygiene promotion which mention neither hands nor their hygiene. Of note, it is not national guidance writers’ role to repeat what international IPC organisations say – it is their job to state whether the international organisations presented evidence to confirm their assertions. In summary, WHO got it wrong and everyone else followed suit.
NIPCMs stick with physics defying modes of transmission
The National Infection Prevention and Control Manuals (NIPCMs) across the UK have stuck to their pre-pandemic physics defying mode of respiratory transmission (despite calling the dichotomy between droplets and aerosols “clearly inadequate”). They also omit airborne dispersal as a mode of transmission (I could go on).
The Bak et al IPC multi professional society guidelines have been “archived”. There is no note (as there is with a “retraction”) emboldened on the front cover of these guidelines – they can still be accessed without notification of them having been archived. The recommendations in this guidance are, according to the Healthcare Infection Society (HIS), “no longer valid”. There is no date as to when this happened. They will not be updated – so apparently “guidelines ‘r’ no longer us”. It appears an effective wriggle, no admission of errors, no regret and no remedy. The rationale to change was the WHO changing their definitions in a 2024 document (and even though HIS never used definitions of aerosols or droplets to support their “droplets probable” assertion), the new WHO document was enough to archive the guidance. (My 13 pages of errors submitted twice to HIS was not).
Everyone makes mistakes
Everyone makes mistakes. It was just over 100 years ago that the last text recommended bleeding patients to treat most diseases was published. This was a time when every single doctor’s opinion on treatment was erroneous. Similarly, the IPC guidance production errors discussed above were held to be true by an entire profession contingent on guidance produced by others. Although IPC guidance writers produced policy and affected practice and education everywhere, never in public at least did they go “woops” nor have they investigated how errors happened, nor moved to strengthen what must be either erroneous or erroneously deployed procedures.
Does IPC have a get out of jail free card even when they advocate practice that causes harm?
The higher the level (national / international) guidance production, the more people are reliant on the recommendations, produced by a few, being correct and complete. All IPCTs in the UK are trusting of the few who produce them. As are the Departments of Health who often sponsor them. Yet, there appears no error plan. Widespread consultation is not an effective means to identify errors. Guidance writers don’t effectively look for errors, expect them, admit them, or repair them properly. Just as the WHO and the HIS have done, the guidance writers quietly move on. This is unprofessional, unacceptable and unethical to everyone who relies on them. The credibility of any organisation is enhanced by error prevention and error management. We await some magic “form of words” that will be used by the national IPC guidance writers (and Departments of Health) to morph their physics defying mode of transmission, to one that is evidenced. I hope and await, for some IPC professionals to emerge with credibility and a statement “the way IPC produces guidance must change”, “We apologise for…. “We will become experts in error prevention actively looking for them and having correction plans ready to be deployed should they be identified.” I am ready to support them when they do. In pursuit of truth IPC needs to become experts in error prevention, detection and correction.
Conclusions from R.E.O. Williams Epidemiology of airborne staphylococcal infections review of mechanistic evidence regarding transmission of staphylococci 1966
“The evidence that has been reviewed seems to leave little doubt that airborne transfer can be of importance. It suggests that the acquisition of nasal carriage of S. aureus by patients nursed in hospitals wards if the dose-effect relationship determined experimentally in infants is approximately applicable to adults.”
“Airborne transfer in hospitals gains its special significance… …if a single disperser is potentially able to infect [and or colonise] a considerable number of other patients, who need not be confined within the same room or even perhaps on the same floor…”
Blowers R. Control of infection in hospital wards. PHLS. J. Clin. Path (1961) 14, 18.
“It is remarkable that in many wards where elaborate precautions against staphylococcal infections are taken little importance is attached to the apparently obvious one of removing patients with frank sepsis. Thus, patients who have been admitted with S. aureus pneumonia, empyema, breast and other abscesses, urinary tract infections, septic dermatitis are regularly treated in open wards alongside uninfected patients. Perhaps even more dangerous are those patients who became infected with staphylococci in hospital because the organisms involved are more often epidemic strains and resistant to antibiotics.”